The Great Debate: Leukocytes in Platelet-Rich Plasma (PRP)
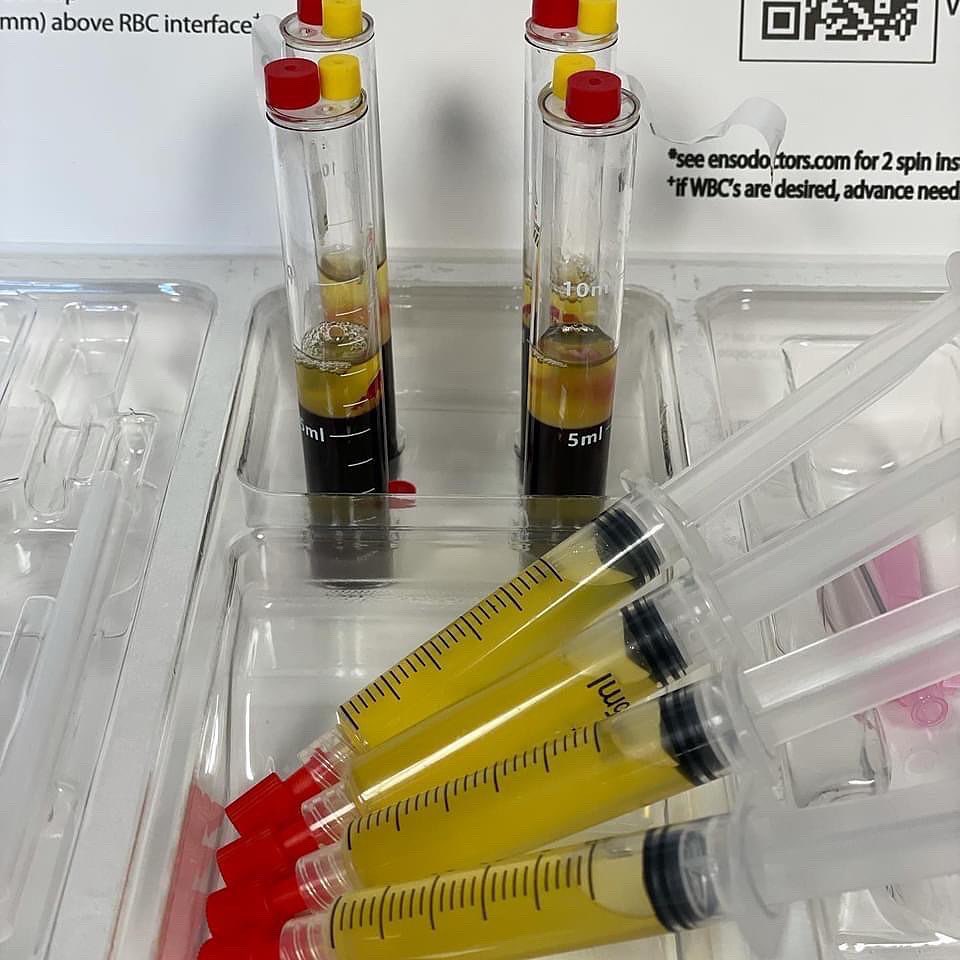
PRP, or Platelet-Rich Plasma, has become a popular tool in regenerative medicine. But achieving optimal results depends heavily on its composition. The most debated element? Leukocytes, also known as white blood cells.
Traditionally, PRP was thought to be better off without leukocytes. The concern was that these cells could trigger inflammation, especially in joints. This led to a preference for leuko-depleted PRP.
However, recent research paints a more complex picture. Let’s delve into the science:
-
Tendon Injuries: A comprehensive review by Fitzpatrick et al. analyzed 18 studies involving over 1,000 patients. Their conclusion? Leuko-RICH PRP, containing white blood cells, showed a stronger association with positive outcomes in treating tendon injuries.
-
Osteoarthritis: The picture gets muddier here. While some studies, like Riboh et al., favored leuko-POOR PRP for osteoarthritis, others observed no significant difference in pain relief. A meta-analysis by Dai et al. even suggested overall PRP outperformed hyaluronic acid, a common osteoarthritis treatment.
The plot thickens with a study by Wakayama et al. They directly compared leuko-rich and leuko-poor PRP for knee osteoarthritis. Their findings? Leuko-rich injections resulted in more frequent and longer-lasting adverse events.
The Takeaway: PRP Isn’t One-Size-Fits-All
The current evidence suggests:
- Tendon Injuries: For tendon issues, leuko-RICH PRP appears to be more beneficial.
- Osteoarthritis: Leuko-POOR PRP might be a better choice for osteoarthritis treatment.
Remember: This is a rapidly evolving field. More research is needed to solidify these findings and explore the optimal composition for other conditions.
The Author: Dr. J. Corey Orava is a leading expert in regenerative medicine. He has extensive experience in designing and evaluating new medical devices, particularly those related to PRP therapy.